Let’s talk design controls – essential, but sometimes overlooked by even established medical device companies.
It’s easy to get excited about a new idea, but it’s far more difficult to ensure that the idea achieves its intended purpose and is compliant with FDA 21 CFR 820.30 and ISO 13485:2016 quality requirements.
These regulations stipulate specific design controls for medical devices. Following these procedures isn’t a mere formality; medical device compliance hinges on applying design controls to ensure that a device:
- Is safe and effective
- Meets the needs of users
- Achieves the intended purpose
- Fulfills specified requirements
Understanding the Regulations Behind Design Controls
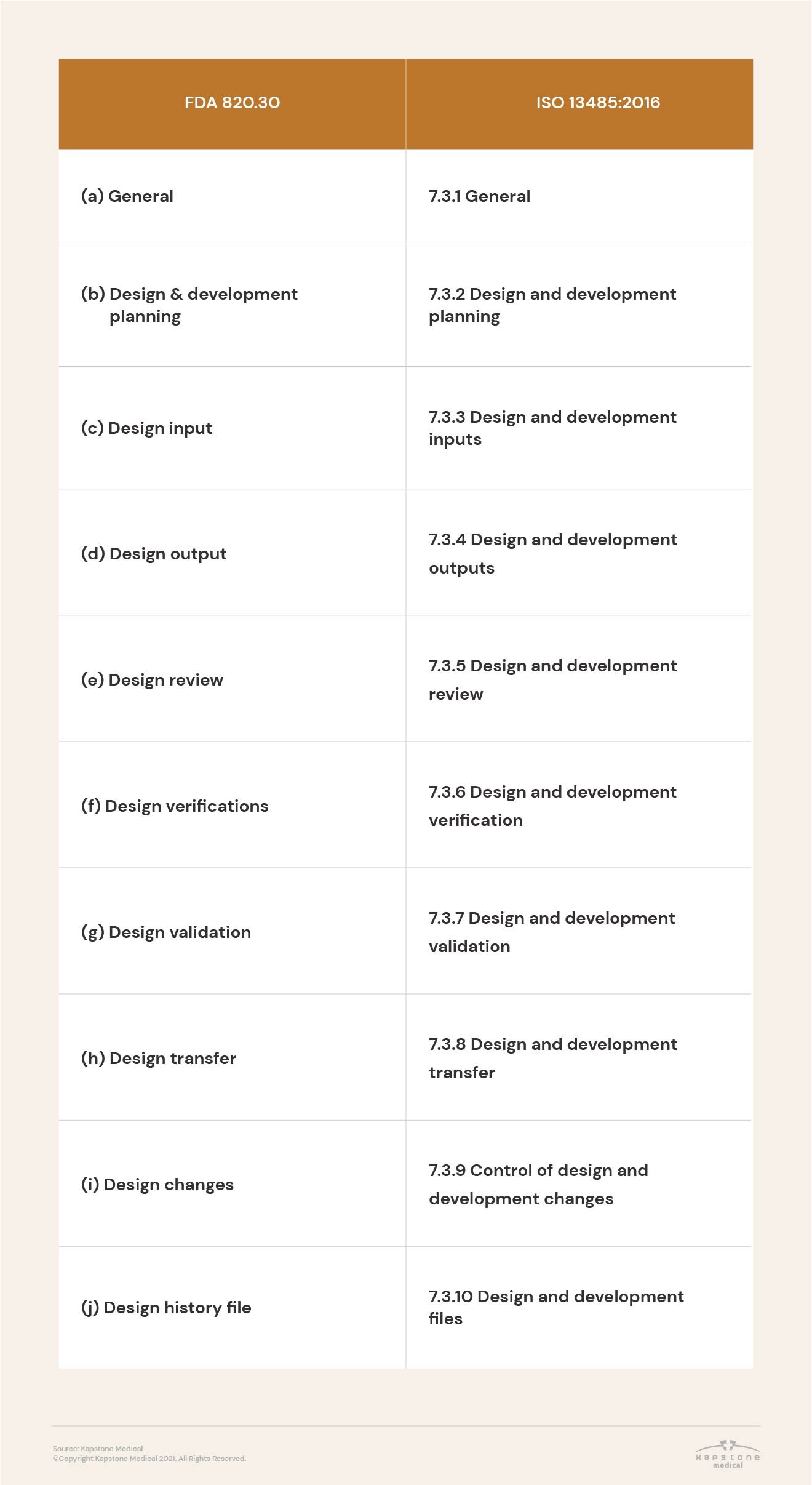
With so much riding on design controls, it’s imperative that medical device companies understand how FDA 21 CFR 820.30 and ISO 13485:2016 align.
Why are these controls so important? Both the FDA and ISO 13485 explicitly require that medical device companies follow a design control process to ensure that their products are safe and effective. You can read about the FDA’s requirements here and the ISO requirements here.
The table below identifies the relevant clauses, which should become the items on your checklist. We’ll go into more detail on each item later in this article.
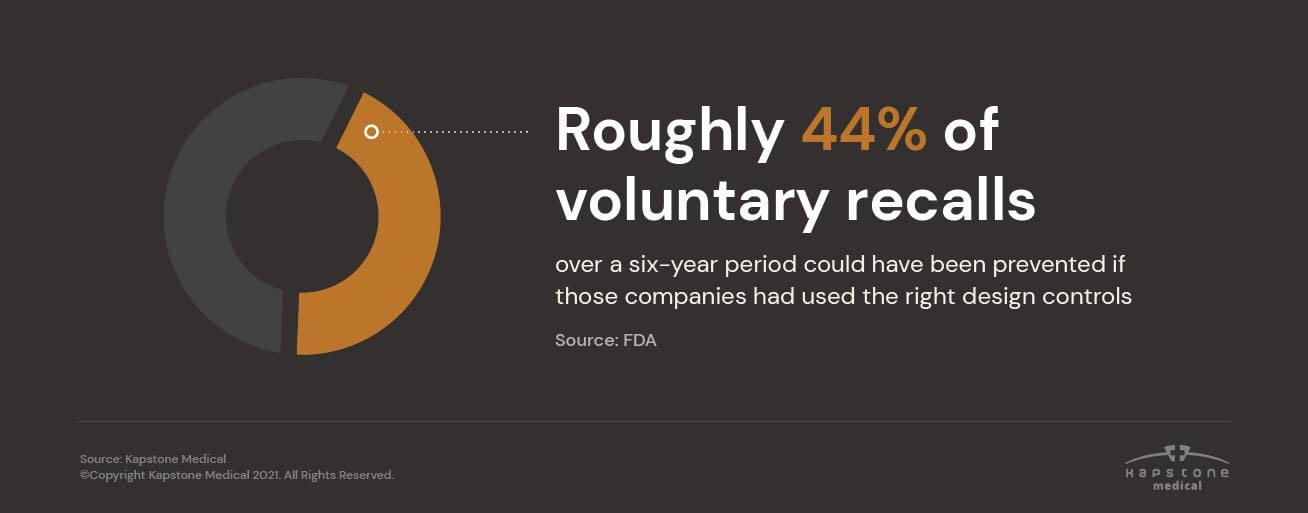
Design controls are also important from a business perspective. The FDA estimates that 44% of voluntary recalls over a six-year period could have been prevented if those companies had applied appropriate design controls. Investing in the right controls related to device design, software, and/or materials and components early in your process can prevent costly consequences down the line.
Assessing “Good” Design Controls and Quality Management
The heart of following good design controls is traceability among all elements, which is typically structured in the format of a matrix.
Traceable: Your system should show every link between inputs, outputs, verifications, validations, and user needs. This process is sometimes referred to as a design control traceability matrix. While it may be cumbersome to create, it can pay massive dividends. If you understand the relationships between your elements, you can quickly address any problems that arise. Plus, traceability is an explicit requirement under ISO 13485. Effective, compliant design controls need to account for risk in order to ensure maximum protection and safety for end users.
Risk-conscious: Keep risk management in mind as you work through design controls. Throughout the process, evaluate what steps are being taken to mitigate risk and if adjustments are needed. Review reporting practices and how they support risk management.
Know Which Medical Devices Need Design Controls
The first question to ask when developing a new medical device is not always a straightforward one. Not all medical devices in the United States require design controls.
Section 820.30 (a) of FDA 21 CFR 820.30 explains which devices need controls, specifically:
- Each manufacturer of any class III or class II device, and the class I devices listed in paragraph (a)(2) of this section, shall establish and maintain procedures to control the design of the device in order to ensure that specified design requirements are met.
- The following class I devices are subject to design controls:
(i) Devices automated with computer software
(ii) The following specifically listed devices:
Section 868.6810 Catheter, Tracheobronchial Suction
Section 878.4460 Glove, Surgeon’s
Section 880.6760 Restraint, Protective
Section 892.5650 System, Applicator, Radionuclide, Manual
Section 892.5740 Source, Radionuclide Teletherapy
However, just because design controls are not required for a particular device doesn't mean a Design History File shouldn’t be kept. Reach out to the Kapstone team for more advice on this topic.
Understanding Quality Systems
Design controls are just one part of your overall quality management system (QMS). The right system will account for design controls, risk management, document control, records management, and supplier management, to name a few.
While it can be difficult to get a QMS off the ground, it is absolutely worth the investment. Not only is it required by regulatory bodies, but a QMS will help your company achieve its outputs and objectives more efficiently and cost-effectively.
The team at Kapstone can help you decide which QMS aligns with your business model and goals — that could mean implementing an entirely new system or making changes to your existing QMS. Either way, Kapstone has the experience and experts to guide successful outcomes.
Create a Design and Development Plan
Design and development planning is much more specific than creating a project schedule. While scheduling and resource allocation are essential, particularly in the design stage, FDA and ISO requirements have different priorities.
FDA 21 CFR 820.30(b) Design & Development Planning
Each manufacturer shall establish and maintain plans that describe or reference the design and development activities, and define responsibility for implementation. The plans shall identify and describe the interfaces with different groups or activities that provide, or result in, input to the design and development process. The plans shall be reviewed, updated, and approved as design and development evolves.
ISO 13485:2016 7.3.2 Design and development planning
The organization shall plan and control the design and development of the product. As appropriate, design and development planning documents shall be maintained and updated as the design and development progresses.
During design and development planning, the organization shall document:
- the design and development stages
- the review(s) needed at each design and development stage
- the verification, validation, and design transfer activities that are appropriate at each design and development stage
- the responsibilities and authorities for design and development
- the methods to ensure traceability of design and development outputs to design and development inputs
- the resources needed, including necessary competence of personnel
Key Factors of a Medical Device Design and Development Plan
In order to comply with these FDA and ISO requirements, your design and development plan should address the following key factors:
- Identify each design & development stage and the associated activities
- Define responsibility for each activity
- Communicate the resources required for each activity (including both internal team members and external vendors, if applicable)
Keep in mind that it’s normal and expected for design and development plans to evolve over time. Having to change your plan or any associated activities is not a sign that your process is inefficient. Instead, it indicates that you’re learning from your activities and optimizing them over time — the very purpose of medical device design controls.
Collect User Needs
Sources of User Needs (as the name implies) originate from actual users. Various user groups should be considered, including the patient, the physician(s), and any supporting staff that interacts with the device over its lifetime. User Needs are not necessarily captured verbatim from a user. Through interviewing or observing how the device is or will be used, the development team can interpret a User Need.
Establish Design Input Requirements
Set yourself up for success by making your design inputs as comprehensive as possible. Consider the following when establishing them in your traceability matrix:
- User needs
- Product’s intended use
- Product’s intended function
- Marketing requirements
- Competitor characteristics and performance
- Regulatory guidance, especially restrictions
Portability is an example of a design input. If you’d like your device to be portable, you’ll need to define what portable means and identify any characteristics or performance elements that could stand in the way, such as excessive device weight or the need to be plugged in to operate.
Compile Design Outputs
Design outputs are the specifications and instructions that explain how to construct your device correctly. Most will correspond to a specific design input.
To use our portability example from above: if portable is the input, the output would be material and construction specifications that make the device portable.
Design outputs may also include the inspection or quality plans that ensure the specification is being met during production.
Device Master Record
Design outputs can be compiled into your product’s Device Master Record (DMR). Think of the DMR as the “ingredient list” for how to manufacture your device in accordance with your inputs. A third party should be able to use the DMR to construct your exact product.
Conduct Design Reviews
Each design review is a formal opportunity for your team to apply your design controls and pivot if needed. This is the time to ask your core design control questions: is your product designed to meet your users’ needs? Is it effective? Are inputs matching up with outputs?
There is no official requirement for when to conduct these reviews or how many you will need to have. We suggest scheduling a review at the completion of each major stage (e.g., user needs identification, design inputs, etc.). Always ensure that the right team members can attend, plus an independent reviewer with little to no stake in that particular review item.
Perform Design Verification Tests
Design verification ensures that the device was designed correctly – that it meets design inputs and performance requirements. The FDA describes this process as “confirmation by examination and provision of objective evidence that specified requirements have been fulfilled.”
Design Verification Best Practices
- Clearly define what your device needs to do and the steps required to achieve that intended purpose
- Define the optimal conditions for your device, how those conditions might change, and how your device will need to adapt (if at all)
- Create inputs that are clear, discrete, actionable, and testable
Perform Design Validation Tests
Validation asks a very different question than verification does. The point of design validation is to determine whether developers designed the correct device. Or, as the FDA puts it, “Validation means confirmation by examination and provision of objective evidence that the particular requirements for a specific intended use can be consistently fulfilled.”
Design Validation Best Practices
- Conduct validation activities on initial production units (units built in your production environment by typical production personnel using design outputs as a guide)
- Test your device in the clinical setting with its intended end user
- Test your device in its specific, intended conditions (including conditions that may change)
- Keep your records organized
Complete Design Transfer
Design transfer is the formal, final handover from development to production. Regulatory submissions should also happen during this period.
In the US: If you plan to submit a 510(k) premarket notification for clearance, you can typically do so once your design verification is complete. Devices that will require premarket approval (PMA) can be submitted at the completion of design validation.
Outside the US, regulatory filings (like CE Mark technical files in the EU) can take place after design validation is complete.
Document Design Changes
Whether adjusting your material composition to achieve an intended input or changing a device’s packaging after clinical testing, design changes are a normal and expected part of the development process. Carefully documenting those changes must be, too.
The FDA specifically requires that “each manufacturer shall establish and maintain procedures for the identification, documentation, validation or where appropriate verification, review, and approval of design changes before their implementation.”
Maintain a Design History File
As a part of your regulatory submission and to prepare for any future audits, you will need to create and maintain a comprehensive design history file. This file should show:
- All design controls and supporting documentation
- Linkages and relationships between design controls (traceability matrix)
- Proof that the device was designed in accordance with controls
- Documentation of changes and impact
- Design transfer materials
Design History File vs. Device History Record
The design history file (DHF) is not the same thing as another document known as the device history record (DHR). The difference is clear in the first word of each name: design vs. device. DHF should include everything that is relevant to the design of your device, while your DHR should include everything that is relevant to the design, development, and production of your device.
In other words, the DHR contains everything you did to make the device and all the instructions a third party would need to manufacture that same device according to its specifications.
Launch Your Medical Device
After completing the design checklist and securing all the necessary regulatory clearance and/or approvals, you should be ready to launch your device in your chosen market or markets.
But, getting to this exciting and much anticipated moment takes a lot of effort. Make the most of your time and resources to get to market faster by collaborating with Kapstone Medical. As a single-source solution, we take a fully integrated approach to new product development, as detailed in our New Product Development (NPD) Roadmap. Click the link below to download your copy of this informative resource.




