A Conversation with Kellen Hills | Regulatory Affairs Specialist, Kapstone Medical
Since 1906, the US Food and Drug Administration (more commonly known as the FDA) has protected consumers against the threat posed by adulterated, mislabeled, unsafe, or otherwise ineffective food and drug products. Regulatory affairs consultant Kellen Hills notes that before the FDA was empowered to regulate these products, “people were getting sick and dying because of unsavory characters putting things out on the market, making false claims about what they did with no oversight.”
While these bad actors, sometimes referred to as “snake oil salesmen,” are still around, it is much harder for them to find a market for their products—all thanks to the FDA’s governance.
The FDA has evolved substantially since its founding, adjusting regulations to account for near-tectonic shifts in the technological and manufacturing landscape. Medical devices, for instance, look a whole lot different in 2020 than they did in 1906 or even 1976, when an amendment to the Federal Food, Drug, & Cosmetic Act first classified devices into three categories, each subject to specific regulatory governance. These classifications still stand, but it is vitally important for medical device companies to stay apprised of the latest requirements within each category, particularly as they look to introduce new devices into the marketplace.
Regulatory clearance for a new Class II medical device requires a 510(k) submission to the FDA. These submissions are complicated, and may seem like a significant barrier to entry for some biotech and device companies. But, as Kellen Hills explains, thorough regulation of these products “is why the FDA was founded in the first place.” These measures are vital to the preservation of public health.
We recently sat down with Kellen to discuss the basics of 510(k) submission, paying special attention to its central requirement: proving substantial equivalence. Here, we cover those basics, dig deeper into substantial equivalence, and clarify the role a regulatory consultant can play in helping your team get a product over the regulatory finish line.

Understanding the Basics of a 510(k) Submission
This may be familiar territory for many of our readers, so we’ll skim over some of this content. In the event that you need more information, you can always get in touch. We’ll connect you to a Kapstone consultant like Kellen who can answer your questions and even assist in the regulatory submission.
Purpose: As Kellen explains, the primary purpose of a 510(k) submission is to “notify the FDA of your intent to market a Class II device in the United States.” The FDA classifies medical devices into three categories based on perceived level of risk, and determines the submission documentation required on that basis. Only Class II devices, which represent a medium level of risk to the consumer, require a 510(k) submission.
Structure: 510(k) documentation should be provided in a “standard format,” Kellen says, “regardless of the type of product. Whether you’re sending a Class II total hip replacement or an ECG device, the FDA likes to see the general sections included.” A typically-formatted 510(k) has twenty-one sections, but sections can be left blank if they do not apply to a particular product. For example: the standard form includes a section on software, but many medical devices (mechanical implants, for one) do not have a software component. In those cases, that section can be left blank.

Substantial Equivalence: The Central Requirement of a 510(k) Submission
Kellen argues that substantial equivalence “is the whole reason that the 510(k) program exists,” and that’s with good reason. When the FDA initially categorized devices into classes in 1976, they actually based those categories on an existing list of devices. Their goal was to streamline future device approvals, as companies that could prove substantial equivalence—in other words, that their device was practically equivalent to an existing, approved device—could secure regulatory approval on that basis without conducting further safety and efficacy trials. In fact, Kellen says, “every Class II product sold in the United States today can trace its lineage back to a product that was on the market in 1976.”
Kellen offers a great example to illustrate how the FDA evaluates substantial equivalence:
Say you have a blue pen, and you want to change it to black. Okay, you can argue that you still hold the black pen in your hand. You still click the button to get the ballpoint to come out. Those features are very similar; the only difference is the color of the ink. Changing the color of the ink does not cause any issues related to the pen’s safety or performance.
Substantial equivalence, as shown in this example, is not a question of aesthetics or other literal, face-value comparisons. It is a question of performance, safety, and results. Proving equivalence on that basis is “basically what you do every time, whether your product is an insulin pump, reusable instrument, implantable plate, or any other device.” A 510(k) needs to demonstrate that while a new product may have new features, those features—and the product’s overall function—are still substantially equivalent to products already on the market.
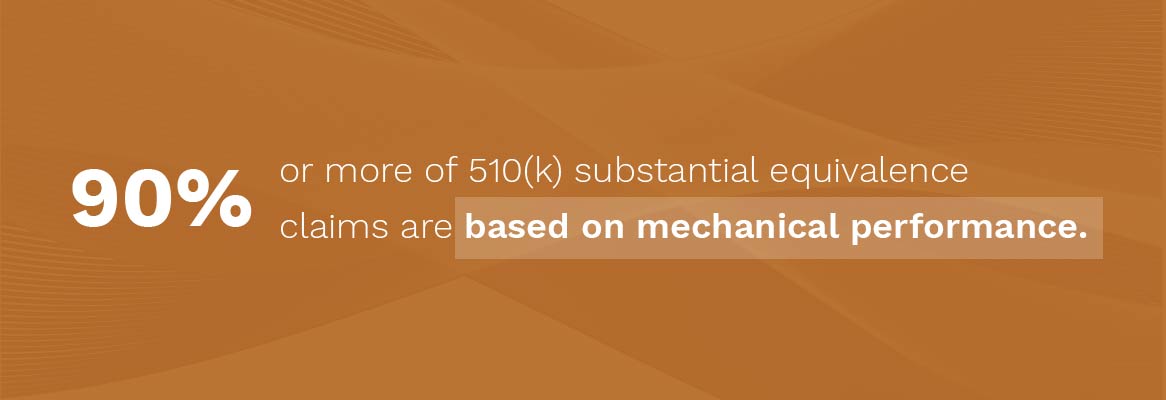
Product mechanics are an essential component of proving substantial equivalence. Kellen estimates that “90% or more of 510(k) substantial equivalence claims are based on mechanical performance,” as it’s relatively straightforward to test how a product works. “If you test two products in the same fashion,” he says, “and do a head to head comparison of their mechanical performance, the same or very similar results demonstrate that those products are, at least in terms of mechanics, substantially equivalent.” Applicants can and should utilize other sections of the 510(k) to discuss other points of equivalence, such as technological characteristics and product design. However, “the meat of the document is going to be the testing of that product.”
It is also worth emphasizing that new devices should have the same patient profile as their predicate devices. Kellen notes that “to be a predicate, a product must have not only the same technological characteristics and mechanics, but also the same or substantially similar intended use.” For example: a screw designed for the bones of the hand should rely on a predicate that is also intended for use in small bones—and not, for example, the femur.
Finally, 510(k) submissions must certify that the predicate product has not been subject to a design-related recall. In Kellen’s opinion, this is a positive guideline. “It forces new manufacturers to stay abreast of changes in technology,” he says. “They can’t necessarily go back to a product that was developed in 1976, because they’d be missing out on forty-five years of product innovation.” Utilizing the latest technology while still observing tried-and-tested guardrails is, in the world of medical devices, a recipe for delivering the best and most effective solutions to patients in need.

When to File A 510(k) Submission And How A Regulatory Consultant Can Help
In past years, the FDA was known to accept 510(k) filings early in product development. The idea, Kellen explains, was to “get their input as soon as you had your concept, some drawings, maybe, and ideally testing.” However, they now require device companies to submit their filings much further along in the process. The FDA expects to see a much fuller picture of a product’s development, including (but not limited to) packaging studies, manufacturing plans, cleaning validations, and other assurances that were previously only a part of quality system regulation (QSR).
The onus to produce this extensive documentation falls on medical device companies, many of which do not have exposure to the world of regulatory affairs and approvals. Some, Kellen notes, do not even have internal regulatory affairs personnel. Given the evolving nature of FDA governance, as well as the many steps required to prove substantial equivalence and earn 510(k) clearance, we recommend that companies strategically outsource this responsibility to regulatory experts.
Kapstone regulatory consultants are equipped to guide, manage, or fully take over 510(k) submissions in the United States (and technical files in the EU), including preparation and submission of all necessary documents. These submissions do not need to be a barrier for medical device companies. With our assistance, you can trust that your device is in the hands of experts with decades of experience and familiarity with the latest regulatory guidelines.
Is your product substantially equivalent to a predicate? What’s missing from your 510(k) submission documents? We can help.


